Let’s be honest. You feel like you’ve tried everything. The cleansers, the expensive serums, the diet changes… yet those stubborn little bumps on your forehead, chest, or back just won’t budge. If traditional acne treatments have failed you time and time again, you might not be dealing with regular acne at all. It’s time we had a straight talk about its tricky cousin: Fungal acne.
So, What Exactly Is ‘Fungal Acne’?
Right, let’s clear this up immediately. “Fungal acne” isn’t actually acne.
It has nothing to do with the bacteria, oil, and dead skin cells that cause traditional spots. The proper medical name is Pityrosporum Folliculitis (or Malassezia Folliculitis), which is just a fancy way of saying you have an overgrowth of yeast in your hair follicles.
Everyone has this yeast on their skin. It’s normally harmless. But sometimes, things get out of balance, the yeast has a party, and you end up with an army of annoying, itchy little bumps.
How to Spot the Difference: Fungal vs. Bacterial Acne
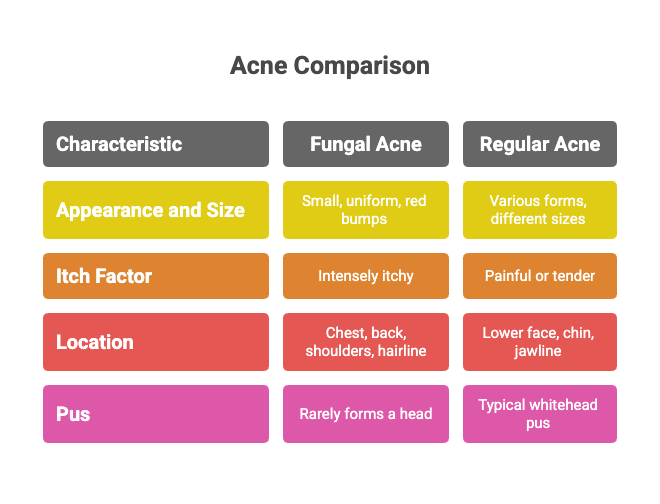
This is the crucial bit. Knowing what you’re up against is half the battle. Regular bacterial acne and fungal acne look and feel very different.
Here’s the breakdown:
- Appearance: Fungal acne bumps are typically very uniform in size – almost like tiny pinpricks or seeds under the skin. Regular acne comes in all shapes and sizes (blackheads, whiteheads, painful cysts).
- The Itch Factor: This is a huge clue. Fungal acne is often intensely itchy. Regular spots can be sore and tender, but they rarely have that maddening itch.
- Location, Location, Location: It loves oily, sweaty areas. Think forehead (especially along the hairline), chest, upper back, and shoulders. Regular acne is more common on the face, like the cheeks and jawline.
- The Squeeze Test: Fungal acne bumps rarely form a “head” and usually don’t contain the classic pus you’d expect from a spot. They are firm little bumps.
What Triggers This Yeast Overgrowth?
Your skin’s environment is key. This yeast thrives in specific conditions. The main culprits are:
- Sweat & Humidity: A long session at the gym or a hot, humid day creates the perfect breeding ground.
- Tight Clothing: Non-breathable fabrics trap sweat and heat against your skin.
- Antibiotics: Sometimes, antibiotics taken for other issues can wipe out the good bacteria on your skin, allowing this yeast to take over.
- Heavy Skincare: Thick, oily moisturisers and suncreams can feed the yeast.
Your Action Plan: How to Get Rid of It
You don’t have to live with it. The treatment is completely different from regular acne, which is why your old routine wasn’t working.
Step 1: The At-Home Fix (A surprisingly simple start!)
The secret weapon for many is an anti-dandruff shampoo. Seriously. Look for one containing an anti-fungal agent like Ketoconazole.
- How to use it: Apply a thin layer to the affected area (like a face or body mask), leave it for 3-5 minutes, and then rinse off. Do this a few times a week.
- Why it works: It directly targets and reduces the yeast on the skin.
Step 2: When You Need the Professionals
If the shampoo isn’t cutting it or if you have a severe case, it’s time to get expert help. At our clinic, we don’t guess; we diagnose. We might recommend:
- Prescription-strength anti-fungal creams.
- Oral anti-fungal medication to tackle the problem from the inside out.
The goal is to get you clear, fast. If you’re tired of the guesswork, book a consultation with one of our skin specialists at Derma Clinic Kathmandu and let’s create a plan that actually works for you.
Frequently Asked Questions (The Stuff You Really Want to Know)
1. Can I use my regular acne products on fungal acne? Probably not. Ingredients like Benzoyl Peroxide won’t work, and some antibiotic creams can even make it worse. Stick to gentle cleansers and anti-fungal treatments.
2. Does diet affect fungal acne? The link isn’t as strong as with regular acne, but some people find that high-sugar or high-yeast diets can be a trigger. It’s about finding what works for you.
3. How long does it take to clear up? With the right treatment, you can see a significant improvement in just a few weeks. Consistency is everything.
4. Can fungal acne come back? Yes, it can. Because the yeast lives on our skin naturally, flare-ups can happen if the conditions are right (e.g., you start going to the gym more, or in the summer months). Maintenance is key.
5. Is it contagious? No. You can’t “catch” it from someone else. It’s your own skin’s yeast overgrowing.
6. What kind of moisturiser should I use? Look for oil-free, lightweight, non-comedogenic formulas. Some heavy oils (like coconut oil) can feed the yeast, so it’s best to avoid them on affected areas.
7. Should I pop the bumps? Absolutely not. There’s nothing to “pop,” and trying will only lead to inflammation, irritation, and potential scarring.
8. Why did I suddenly get this now? It could be anything! A course of antibiotics, a new fitness routine, a stressful period, or even a change in the weather. The trigger isn’t always obvious.
The Bottom Line
Understanding that you’re fighting a yeast, not bacteria, changes the entire game. Stop wasting money on products that will never work and start tackling the real root of the problem. With the right knowledge and a targeted approach, you can get clear, calm skin. For more personalised advice, Please Visit Derma Clinic and Consult with dermatologist . We offer a wide range of effective fungal acne treatment options.


